Heading to the doctor? Take The GERD Doctor Checklist.
So many of my patients struggle with a condition called Gastroesophageal reflux disease (GERD).
According to statistics, 20% of the U.S. population suffers from diagnosed GERD with upwards of 40% complaining of GERD-like symptoms at least once a month. (1,2) This is a chronic condition that causes daily heartburn, acid reflux and other frustrating symptoms. Although not a life-threatening condition in most cases, GERD can cause serious problems if left untreated. There are many conventional and natural treatments for GERD. Most of my patients use a mixture of both short-term drug therapy and long-term lifestyle changes. With knowledge and committed action, I believe most people can overcome symptoms of GERD and live a healthy life free of heartburn and other obnoxious symptoms.
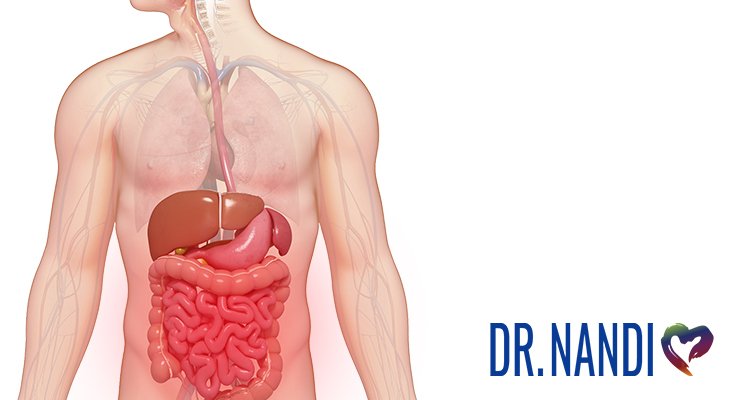
What Is Gastroesophageal Reflux Disease (GERD)?
Gastroesophageal reflux disease (GERD) happens when acid and other contents from the stomach frequently come up into your esophagus, causing irritation of the sensitive esophageal lining. GERD is different than occasional heartburn or indigestion as it is chronic and happens at least twice a week and for some people, multiple times a day.
Symptoms Of GERD
- Acid indigestion
- Heartburn
- Painful burning sensations in the throat/chest
- Bad breath
- Tooth erosion
- Abdominal pain
- Chest pain
- Asthma symptoms (wheezing, difficulty breathing, especially during exercise)
- Belching
- Bloating
- Regurgitation
- Excessive saliva
- Hoarseness
- A sour taste in the mouth
Are GERD Symptoms Constant?
If you have true GERD and not just irregular heartburn/indigestion, you will experience several symptoms of GERD daily or several times a week. If this is the case I would recommend scheduling an appointment with your doctor so that you can come up with a plan that best meets your unique situation and needs. There are many things you can do to help relieve symptoms of GERD. You don’t need to suffer long term.
GERD vs. Acid Reflux/Silent Reflux
Acid reflux and GERD are very similar but don’t necessarily mean the same thing. When you experience acid reflux, regurgutated food or sour liquid from your stomach flows up into your esophagus, causing heartburn or pain in the throat. Most people experience this on occasion due to spicy food or abnormal movement after eating (laying down immediately or the head being slanted downward). GERD is a disease, where acid and contents from the stomach come up frequently. This can lead to damage of the sensitive lining of the esophagus and cause many other symptoms besides heartburn (listed above).
Who Is At Risk For GERD?
There are several factors that may contribute to one developing GERD. Anyone can develop this condition, including men, women, infants and children. Following are the most common underlying problems that lead to a GERD diagnosis:
Untreated Food Allergies
A food sensitivity, intolerance or allergy that goes untreated for a long period of time leads to poor gut health which can develop into Leaky Gut Syndrome or IBS. As mentioned above, these conditions are frequently accompanied by acid reflux and GERD.
Hiatal Hernias
The hiatus is an opening between the diaphragm and the abdomen. The esophagus is inside this opening; connecting the stomach and the mouth. A hiatal hernia causes the stomach to bulge into the chest, causing severe heartburn.
Obesity
A large belly has been shown to cause or worsen heartburn and GERD. (8) A 2006 study found that even relatively small changes in weight can increase the severity of acid reflux disease and risk for complications. (13) This is thought to be because excess weight puts additional pressure on the abdominal region, making acid leakage more likely. Obesity may also cause inflammation in the body, which is associated with GERD symptoms.
Inflammation
Medical professionals use to blame excessive acid production in the stomach and acid reflux as the only causes of GERD. New research has found that while excess acid production does play a role, chronic inflammation may also be a major contributor to the disease. (7) Although inflammation in moderate amounts is healthy and appropriate, sometimes the body gets “stuck in high gear”, either because it failed to eliminate whatever was causing acute inflammation or because of an autoimmune disorder. When this happens, inflammation becomes chronic and can lead to a variety of health issues and symptoms, including GERD.
Physical and Emotional Stress
Chronic stress leads to inflammation which leads to chronic disease. Too much stress also contributes to poor sleep, weight gain and poor nutritional choices. A 2009 study involving over 40,000 Norwegians found that people who had more work-related stress were at greater risk for developing GERD symptoms. (14)
Sedentary Lifestyle
Studies have found that a sedentary lifestyle, along with obesity and acid reflux, are linked to GERD and more GERD related complications in the elderly. (9)
Smoking Cigarettes
Nicotine relaxes the ring of muscle in the lower esophagus that is responsible for keeping acid in the stomach, thus making it easier for said acid to travel up into the throat.
A Diet High In Acidic, Processed and Refined Foods
There are many foods in the Standard American Diet that aggravate the digestive system. Overconsumption of these foods, for many people, eventually leads to digestive issues including acid reflux and GERD.
Foods That Aggravate GERD
- Caffeine. Caffeinated drinks irritate the esophagus and weaken the esophageal sphincter.
- Alcohol. Especially when consumed close to bedtime, alcohol often contributes to symptoms of GERD.
- Spicy foods. Spicy foods are a big culprit for many of my patients with acid reflux. Avoid spicy foods until your symptoms are improve.
- High-sodium foods. Like processed foods and fast foods.
- Fatty and fried foods.
- Citrus.
- Chocolate. An ingredient in chocolate called theobromine relaxes the esophageal sphincter and increases reflux.
- Foods you are allergic to. I suggest working with your doctor to determine foods you may be sensitive/intolerant to so that you can remove them from your diet. These may include processed dairy products, grains, gluten, eggs, nuts, synthetic ingredients, food dyes, etc.
Am I At Risk?
If you want more information about GERD, as well as a self-diagnosis quiz designed to help you know if you should bring symptoms up to your doctor, you will soon be able to download my full book: Beating Gerd Naturally- Dr. Nandi’s Guide To Managing GERD. This book also contains my full protocol for managing GERD. I always recommend working alongside your dedicated medical professional.
GERD When Pregnant
Many women complain of heartburn and GERD-like symptoms during pregnancy. This may be caused by several factors. Pregnancy hormones slow down the digestive system, including the muscles of the esophagus. As the uterus expands to fit a growing baby, it pushes on the stomach which may lead to acid being forced up into the throat. Luckily, these symptoms rarely last beyond the first or second trimester, and normally disappear entirely once the baby is born.
Treatment For GERD During Pregnancy
For pregnant women experiencing GERD symptoms I recommend first trying lifestyle changes (listed below). If this doesn’t seem to help and symptoms are severe, I suggest non-prescription medications such:
- Chewable antacids made from calcium carbonate
- Antacids containing magnesium hydroxide or magnesium oxide
When pregnant, is important to avoid medications containing:
- Aluminum (aluminum hydroxide, aluminum carbonate)
- Aspirin (i.e. Alka-Seltzer, salicylate, acetylsalicylic acid)
If your GERD is severe, then ask your doctor if stronger medications are safe for you.
GERD in Infants and Toddlers
GERD can occur in infants and children due to an immature gastrointestinal tract. Although most babies and children grow out of GERD, the symptoms can be uncomfortable and disrupting while they last.
Common symptoms of GERD in infants and children are:
- Projectile vomiting (more intense than normal baby spit up)
- Persistent cough
- Wheezing
- Difficulty eating (choking, gagging)
- Refusal to eat
- Gas, colicky behavior (especially after feeding)
- Regurgitation and re-swallowing
- Complaining of a sour taste in their mouth (especially in the AM)
- Recurring pneumonia
Most infants with GERD are completely symptom-free by age 1. Only 5% of these babies continue to have symptoms as toddlers. (6)
Treatment For GERD In Infants
Some natural treatments I recommend for infants with GERD symptoms:
- Hold infants upright for 30 minutes after feedings
- Avoid overfeeding
- Burp infants once in the middle of a feeding and again after
If symptoms persist and cause problems with sleep, feeding and proper growth, I suggest working with the child’s pediatrician to see if a medication might be necessary. Over-the-counter and prescription medications to address infant GERD include:
- H2 blockers
- Proton Pump Inhibitors (PPIs)
How Is GERD Treated In Adults?
When choosing a protocol to tackle GERD symptoms, always work with your doctor to help create the best plan for you and your unique situation. Following are some of the most common conventional and non-conventional treatments used to treat GERD. For a more comprehensive guide, you can download my full book on managing GERD.
Conventional Treatments for GERD
Antacids
Antacids neutralize the acid in your stomach and may provide fast-acting, temporary relief from occasional heartburn, reflux and GERD symptoms. Common over-the-counter antacids include:
- Alka-Seltzer
- Alternagel
- Amphojel
- Gaviscon
- Maalox
- Milk of Magnesia
- Mylanta
- Rolaids
- Tums
H2 Blockers
Histamine 2 (H2) blockers reduce the amount of acid produced in the stomach. These are taken in the morning with breakfast, at night during dinner, or both. Popular H2 blockers include:
- Famotidine (Pepcid, Pepcid AC)
- Cimetidine (Tagamet, Tagamet-HB)
- Nizatidine (Axid, Axid AR)
- Ranitidine (Zantac, Zantac 75)
Proton Pump Inhibitors
Proton pump inhibitors (PPIs) have revolutionized the treatment of GERD. They are the most effective medication available for healing a damaged esophagus. PPIs work by reducing the amount of acid produced in the stomach. Specifically, they work by blocking an enzyme known as the “proton pump” that is found in the wall of the stomach and is involved in producing acid. The pump releases protons into the gastric juices, which become acid. By blocking this enzyme, PPIs decrease the amount of acid produced in the stomach. This lowers the risk of acid spilling out into your food tube, giving your esophagus time to heal. Popular PPIs include:
- lansoprazole (Prevacid)
- esomeprazole (Nexium)
- omeprazole (Prilosec)
- dexlansoprazole (Dexilant, Kapidex)
- pantoprazole sodium (Protonix)
- rabeprazole sodium (Aciphex)
When GERD Requires Surgery
Although uncommon, there are some people who aren’t helped by medication or lifestyle changes. Some patients cannot tolerate the medicines. They suffer from complications from GERD. In these cases, surgery may be a good option to find relief. There are several different types of surgeries that your doctor might consider.
- Fundoplication. This is a standard surgery for severe GERD cases. It essentially tightens the esophageal sphincter, and reinforces it using the upper part of the stomach.
- Transoral Incisionless Fundoplication. This procedure creates a small barrier between the stomach and esophagus, making it more difficult for acid to come up. It doesn’t require any incision.
- Stretta Procedure. This is a fairly new procedure that is performed with an endoscope. Radiofrequency energy is delivered and helps to strengthen the muscle at the end of the esophagus, the LES. Also, this muscle has fewer relaxations, decreasing the amount of acid entering the esophagus.
- Bard Endocinch System. This is another procedure that uses an endoscope. Stitches are made in the esophageal tissue which strengthen the esophageal sphincter.
- Linx surgery. This surgery uses a unique device called a linx, which is a ring of tiny magnetic titanium beads. These are wrapped around the esophageal sphincter to strengthen it. The beads are magnetized and move together to keep the opening between the stomach and esophagus closed. Food can still pass through normally.
Surgery is generally considered a last resort for GERD patients and are done only when medication and lifestyle changes don’t work.
Lifestyle Treatments for GERD
With any medical condition it is extremely important to address your dietary and lifestyle habits. Everything you consume affects your health and wellbeing. Food can be the greatest medicine or it can be poison. Choose what you eat intentionally and with love for your body. Here are some important lifestyle changes to make if you have GERD or acid reflux.

GERD Diet
Whether you choose to take medications for your GERD symptoms or not, you should definitely focus on changing your diet and lifestyle habits to improve your health. There are some specific guidelines I give to my GERD patients that I will share with you here. For a more comprehensive guide, you will soon be able to download my book: Beating Gerd Naturally- Dr. Nandi’s Guide To Managing GERD. Eat More Of THESE:
- Leafy greens
- Vegetables (only raw tomatoes)
- High-quality bone broth
- Ginger and turmeric
- Omega-3 fatty acids
- Lean proteins
- Fruit (except citrus)
Eliminate These:
- Coffee
- Soda
- Energy drinks
- Chocolate
- Fried and fatty foods
- High-fat red meat
- Tomato sauce
- Mint
- Citrus fruits and juices
- Processed dairy
- Spicy foods
- Alcohol
Eat Smaller Meals
Overeating puts more pressure on the stomach and may push acid into the esophagus. Instead of eating 2-3 large meals every day, eat 4-5 smaller meals every three or four hours.
Avoid Nighttime Snacks
Snacks can wreak havoc on your insides if you eat them before going to bed. The following foods especially contribute to heartburn, indigestion and acid reflux if consumed late at night:
- High sugar snacks and sweets (cookies, ice cream, candy, juice)
- Greasy, high-trans-fat foods (fried foods, chips, fast food)
- Spicy foods
- Large meals
I suggest eating snacks that have a little protein and healthy fat. Vegetables and a healthy dip, fruit, some nuts and seeds, a homemade low-sugar dessert, etc. So for those of you suffering with GERD, please snack during the day. Take a look at our free SuperSnack guide for wonderful ideas!
Maintain A Healthy Weight
In a 2012 study published in the journal Obesity, women who lost just 5 to 10 percent of their body weight and men who shed 10 percent of their body weight experienced a reduction in their GERD symptoms. The more the weight lost, the greater the improvement. (10)
Stop Smoking
Studies have suggested that tobacco smoking may be a risk factor for GERD. (11) Nicotine relaxes smooth muscle in the body, including the esophageal sphincter, making it easier for acid to travel up from the stomach into the throat. People who smoke are also more likely to have a chronic cough, which puts constant pressure on the respiratory and digestive systems.
Alleviate Stress
In a 2015 study in Internal Medicine over 12,000 people with GERD said stress was the number-one factor that exacerbated their symptoms. Stress also increases risk of obesity, inflammation and other health-damaging conditions that can cause and/or aggravate GERD symptoms.
Heading to the doctor? Take our GERD Doctor Checklist.
Other Frequently Asked Questions About GERD
Q. Will GERD go away?
A. Many of my patients are able to find relief from GERD after following a personalized protocol including short-term drug therapy and long-term lifestyle changes.
Q. Will GERD go away on its own?
A. If one doesn’t make lifestyle changes to address GERD symptoms, it is unlikely it will go away on its own. However with some simple habit changes, and medication for severe cases, most people find long term relief from GERD.
Q. Can GERD be cured permanently?
A. Although GERD cannot be “cured”, it can be effectively managed and symptoms nearly eliminated with committed action and the help of a professional.
Q. Will GERD cause chest pain?
A. Non-cardiac chest pain is a symptom of GERD. If you have GERD and are experiencing chest pain, it can be due to esophageal spasms which are the result of acid damage from reflux.
Q. Can GERD cause back pain?
A. Some of my patients complain of back pain and it is indeed a symptom of the GERD.
Q. Can GERD kill you?
A. GERD on it’s own is not considered a lethal disease. But left untreated long-term, GERD can lead to serious complications like esophageal cancer and Barrett’s esophagus which can be much more dangerous and even deadly.
Q. Will GERD cause asthma/difficulty breathing?
A. 75% of adults with asthma also have GERD. (4) It isn’t completely clear why GERD may trigger asthma symptoms, but researchers believe it may be due to damage of the esophagus and airways from stomach acid. On the flip side, asthma may also exacerbate and trigger symptoms of GERD, due to the lungs swelling during an asthma attack and putting pressure on the stomach.
Q. Where is GERD pain felt?
A. GERD pain may be felt as a burning sensation in the throat, tightness and pain in the back and even chest pain (heartburn).
Q. Which side to sleep on with GERD?
A. Several studies have shown that sleeping on your right side aggravates heartburn, and sleeping on the left calms it. (5)
Q. Which doctor treats gerd/Who diagnoses gerd?
A. A general doctor may diagnose GERD based on a physical examination and history of symptoms. For a more accurate diagnosis and treatment, you may be referred to a gastroenterologist.
Q. Are GERD and gallstones related?
A. GERD pain and gallbladder pain can feel similar, but these conditions are different and generally not related. While the symptoms of GERD such as heartburn and acid reflux come and go, most gallbladder pain gets sharper and more painful over time.
Q. Are GERD and gastritis the same?
A. Gastritis is inflammation in the stomach lining. It is possible to have both GERD and gastritis at the same time but they may also occur separately.
Q. Are GERD and anxiety related?
A.Studies have found that that GERD patients are more likely to suffer from anxiety and depression than healthy patients. (12)
Q. Are GERD and indigestion the same thing?
A. Indigestion is a condition of impaired digestion that may cause upper abdominal fullness, nausea, heartburn, or abdominal pain. Indigestion can often be a symptom of an underlying problem such as GERD.
Q. Are GERD and sleep apnea related?
A. Some researchers believe that GERD may cause obstructive sleep apnea, because of the vocal cords spasming due to refluxed acid. Others believe that obstructive sleep apnea causes GERD by causing airway pressure changes that make reflux more likely during sleep.
Conclusion
If you think you might have GERD, I suggest scheduling an appointment with your healthcare professional. Here is a Doctor Visit Checklist to help you have the most productive visit possible.
To learn more about this condition and how to effectively treat it, you will soon be able to download my 60-page guide: Beating Gerd Naturally- Dr. Nandi’s Guide To Managing GERD. I believe strongly that we all should be our own #HealthHero. This means that we are committed to our wellbeing and will do what it takes to live a life of health and vitality. When you feel your best, you can make the most impact in the lives of those you love and in the community you live in.
Did you find the information in the post useful? What other conditions would you be interested in learning about on our blog? Comment below.
References
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4133436/
- https://www.ncbi.nlm.nih.gov/pubmed/24811245
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2839176/
- http://my.clevelandclinic.org/health/diseases_conditions/hic_gastroesophogeal_reflux_disease_GERD/hic_GERD_and_Asthma
- https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/410292
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1395762/
- https://www.ncbi.nlm.nih.gov/pubmed/10566710
- http://www.obesityaction.org/educational-resources/resource-articles-2/obesity-related-diseases/obesity-heartburn-what-is-the-link
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3010469/
- http://www.obesityaction.org/educational-resources/resource-articles-2/obesity-related-diseases/obesity-heartburn-what-is-the-link
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2668774/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4394093/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2921086/
- http://informahealthcare.com/doi/abs/10.3109/0036552090340167